Financial Incentives are Only Part of the Strength of Physician Alignment
Seems everyone is talking about physician alignment. In March 2014, Tom Atchison presented at ACHE’s Congress (2014) the session: “Physician Alignment: Dos and Taboos.” Atchison reinforced to attendees to make sure to not call employed physicians “owned”. He reflected that just because a health system
pays a doctor’s salary, it does not mean that the physician will comply in all processes. Money is not the sole motivator…for physicians as with anyone else. Atchison stressed the need to have a shared vision with common incentives.
I thought about Atchison’s presentation when I read “Physician Clinical Alignment and Integration: A Community-Academic Hospital Approach” (Salas-Lopez, Weiss, Nester, & Whalen, 2014). The authors contrast the unsuccessful alignment strategies of the 1990s with efforts that are “mutually beneficial, driven by the need to achieve better care coordination, increased access to infrastructure, improved quality, and lower costs.”
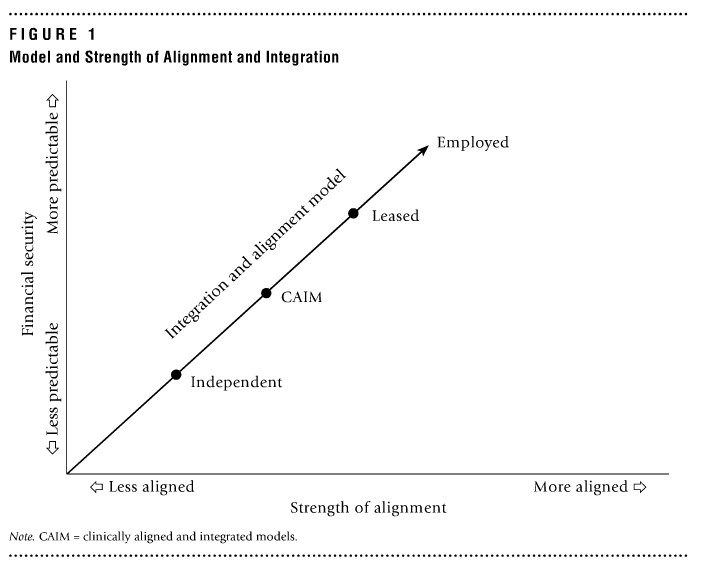 My disagreement with the authors is in their “model” depicted in Figure 1 that shows a perfect relationship between financial security with strength of alignment between physicians and hospitals. The authors propose that the degrees of alignment and integration are based on the extent of financial security.
My disagreement with the authors is in their “model” depicted in Figure 1 that shows a perfect relationship between financial security with strength of alignment between physicians and hospitals. The authors propose that the degrees of alignment and integration are based on the extent of financial security.
The model shows, I believe erroneously, that alignment is perfectly correlated with financial security, with independent physicians being less aligned, followed by “Clinically Aligned and Integrated Models”, then “Leased”, and lastly “Employed” physicians as being the highest level of alignment. Their model makes an overly simplistic judgment – that employed physicians are highly aligned. The model is in sharp contrast to the core of their article which talks about prioritizing cultural compatibility and setting clear expectation for achieving shared goals and ideals. They even reference that clinical alignment and integration agreements may appeal to independent physician groups who wish to retain moderate autonomy.
Atchison would argue that you can have employed physicians who are poorly aligned, and independent groups who are highly aligned. Alignment can occur over all levels of employment, even with independent physicians.
Gainsharing can serve as a conduit to align physician and hospital goals. Hospitals and the medical staff are misaligned because there are different payment systems that prevent each from reaching their goals. Why? Well, in most cases, hospitals are paid on a case rate, while physicians are paid on a “fee-for-service” basis. In their analysis of the Gainsharing program implemented through the Greater New York Hospital Association at NYU Langone Medical Center (Seligman and Chorney, 2013) find: “The disconnect arises because physicians are reimbursed based on the number of services provided, while hospitals are increasingly being rewarded for achieving high-quality outcomes in the most cost-effective way.” Through gainsharing, Seligman and Chorney found that their hospital realized improved clinical scores, such as a decrease in readmission rates and mortality rates, and a decrease in length of stay and costs.
In the Practitioner Response to the Salas-Lopez article, (Fulton, 2014) emphasizes that “Physician are looking for long-term partnerships where they can participate actively in the transformation of patient care delivery models, provide the most appropriate and highest-quality care, and stabilize their financial future.”
Gainsharing can work with different physician-hospital partnership approaches (employed, leased, independent, etc.). The level of financial relations (employed vs independent) does not matter for the success of the program in meeting cost and quality goals. Gainsharing requires a shared vision of what to accomplish, a buy-in of the medical staff, and a balance of clinical outcomes as gates. These elements are necessary for alignment; a financial contractual relationship does not automatically create alignment.
References
Atchison, T. (2014). Phyisician Aligment: Dos and Taboos. American College of Healthcare Executives Annual Congress. Chicago.
Fulton, M. S. (2014, May/June). Practitioner Application (Physician Clinial Alignment). Journal of Healthcare Management, 59(3), 208-209.
Salas-Lopez, D., Weiss, S., Nester, B., & Whalen, T. (2014, May/June). Phyisian Clinical Alignment and Integration: A Community-Academic Hospital Approach. Journal of Healthcare Management, 59(3), 195-209.
Seligman, D., & Chorney, G. S. (2013, August). Aligning Physician and Hospital Goals through Gainsharing. Retrieved May 29, 2014, from American Association of Orthopaedic Surgeons: http://www.aaos.org/news/aaosnow/aug13/managing5.asp

Title: Research Specialist
Organization: American Hospital Association/Health Research & Educational Trust
Great job with illustrating a clear picture of different elements involved in physician alignment. I agree that financial incentive does not automatically guarantee physician alignment. A shared vision and buy-in of medical staff with balanced clinical outcomes is important to achieve long-term partnerships with physicians to actively participate in the transformation of patient care overall.
[Disclaimer: I work for the AHA but the views expressed here are my personal views.]